Welcome
Please watch this short video introduction from our CEO and Board President.
Exceptional Care
Patient Stories
A Life Saved
Don Bilodeau
Healthier for Surgery
James Warpinski
Hope & Recovery
Charlotte Jackson
{Y}our Tomorrow
Lauri Ellis
Back in Balance
Linda Pelkey
A Life Saved
Don Bilodeau

Don Bilodeau doesn’t remember the day he died or being brought back to life.
His wife sure does, though. It was an experience she’ll never forget … one that includes the sight of Don, lifeless next to her in her car, and the team at NMC working hard to bring him back.
That Sunday started typically for the Montgomery couple; Don and Christina had breakfast together and she went off to work at an apartment building they own. Don showed up mid-morning and said he didn’t feel well. He was tired, rested for a bit and then, unexpectedly, asked Christina to take him to the hospital.
Christina knew something must be serious for him to make that request and so they got right in the car and began the 40-minute drive to St. Albans. He didn’t complain of chest pain or shortness of breath, just tiredness and a bit of nausea. Suddenly, though, he made an odd noise and she watched him arch his back, clench his fists and stop breathing. Thus, began one of the most frightening experiences of her life.
She immediately began chest compressions with one arm as best she could as she drove madly the rest of the way along Route 105 to Fisher Pond Road. They got lucky with light traffic, a green light, and no approaching traffic when they passed a milk truck, eventually arriving at NMC blaring the horn.
Christina ran inside, and nurse Kari-Ann Tremblay ran back out with her along with Dr. John Minadeo, NMC’s Chief Medical Officer and an ED physician. The two started CPR, got Don on to a stretcher, and with more help from the team, got him inside. Luckily, Don’s heart was in a rhythm that allowed Dr. Minadeo to shock him with a defibrillator and get his pulse back.
That kind of quick response isn’t unusual for the ED team, said Dr. Minadeo, praising the department’s staff who are highly-trained, quick-thinking and compassionate. What is unusual, he said, is to have a positive outcome from this kind of case.
Christina was surprised that she was allowed into the room where the team was at work, trying to revive her husband. A nurse stayed at her side, explaining what the team was doing. “It was just amazing to watch this,” she said. He lost his pulse again, and again the team shocked him to re-start his heart.
Don had had a heart attack and had a very weakly pumping heart – a very dangerous situation. Despite losing his pulse again, the NMC team stabilized Don, started therapeutic hypothermia and transferred him to the University of Vermont Medical Center. There he required two procedures, one combatting artery blockages, and the other to insert a balloon pump to assist the beating of his heart.
At UVMMC, Don flatlined again, was brought back, and Christina continued her worried waiting, hearing from providers that his situation was dire. Following the surgeries, UVMMC air-lifted him in the early morning hours to Massachusetts General Hospital, uncertain that his heart condition could be adequately treated in Vermont if his condition worsened.
Christina drove to Boston with the couple’s nieces Carrie and Dorothy, and spent two weeks there, as Don slowly recovered. Amazingly, he needed no further surgeries and the doctors slowly weaned him off the medications and the balloon pump that was supporting his heart function. At times the healthcare team would allow Don to wake and assess his cognitive function – with encouraging signs.
Only late in his hospital stay does Donnie’s memory return. He vaguely remembers being at Mass General – but nothing before that, dating back to breakfast the day of his heart attack. After a two-week stay, the doctors sent him home. That four-hour drive was only slightly less nerve-wracking for Christina than the first one. “I was pretty much scared to death,” she said.
Don had been receiving IV antibiotics for a mild infection and needed to continue that when he returned home. This brought him back to NMC.
Having come home on a weekend, he was once again treated in NMC’s Emergency Department, this time receiving his antibiotic infusion. Having returned exactly two weeks later, the same team was working in the ED. Dr. Minadeo was shocked to learn that Don was back, and in good health.
“People don’t usually have that type of recovery,” he said. “Lots of fortuitous factors lined up to offer him a successful outcome.”
Don and Christina agreed that good fortune played a big role in his survival – but they are also grateful for the exceptional care they received in all three hospitals, and were impressed by their glimpse into emergency medicine.
For Dr. Minadeo and the ED team, Don’s return visit and good health was welcome good news. “It’s rewarding, and re-affirming, to see these kinds of extreme measures – that aren’t usually successful … really do save lives… and whole families lives,” he said.
Kari agreed that getting to reconnect with Don and his wife was wonderful. ED staff deal with death and dying all the time, she said, and are happy to care for and comfort patients no matter the outcome. But getting the good news of a life saved is uplifting. “This is why we do what we do,” she said.
Happily, the changes for Don and Christina have been simple and positive: a need to take care for a steady recovery, and a deeper appreciation for life … having seen how quickly it can slip away.
Surgical Optimization
James Warpinski

Lifestyle Medicine: A simple formula for success
The formula for weight loss, feeling good, low cholesterol and a healthy blood pressure is actually a simple one. Eat well and be active.
So why is it so difficult for so many people to lead the healthy lifestyle that they want? Well, knowing the answer to a healthy lifestyle and actually living the healthy lifestyle are vastly different things.
Ask James Warpinski, a local mental health counselor, who worked this year with NMC’s Lifestyle Medicine Clinic to lose weight and reduce his high blood pressure. He says he knew that healthy food choices and being more physically active would work … but it was the accountability, encouragement and motivation provided by the Lifestyle Medicine team that helped him put the wellness formula into action and create success.
He was referred to the clinic by surgeon Anna Royer of Northwestern Associates in Surgery. She recommended he lose some weight and address his blood pressure before a surgery that he needed. He was surprised that his blood pressure had gotten so bad, and was thankful that Dr. Royer recommended he take action. “It was the kick in the butt I needed,” he said.
His first appointment at the Lifestyle Medicine clinic set the tone and the foundation for his success. That first, hour-and-a-half-long visit with Dr. Elisabeth Fontaine and Health Coach John Burke focused on his goals, and learning about him, his life and the healthy habits he already had down pat.
He then met every two to three weeks with Wellness Specialist Kate Robinson and Registered Dietician Lindsay Hoar. Those regular check-ins kept him honest. In addition to providing a natural accountability check, James had established a strong enough relationship with the team that he felt he could be totally honest about slips and setbacks.
“They wanted me to succeed,” he said of the Lifestyle Medicine team.
The team recommended he make small changes in his lifestyle – things that he felt sure he could continue. He started walking to work. He began making his own lunch to take to work. He started having a side salad rather than a side of fries. Even small choices – like just one slice of cheese on his sandwich – added up to big impacts.
After 2-3 months, James had lost over 30 pounds and brought his blood pressure down. Just as meaningful were the quality of life improvements. Getting down on the floor to look for something under the couch? No problem. Walking up the two flights of stairs to work? Easy. All combined with a sense of pride in having accomplished what he set out to do.
He recommended the process as a positive one that would benefit many people – especially if the motivation for change is already there. If you have that, he says, Lifestyle Medicine can help. “They’re not going to fix you, you’ve got to fix yourself.”
Hope & Recovery
Charlotte Jackson
Sometimes it is the connection with our families that get us through the toughest experiences. It is certainly that way for Charlotte Jackson who says her two children are her world. “My kids are everything to me,” she says. It was for them that she quit doing drugs, and selling drugs. “I wanted better for them.”
In some ways, it was also thoughts of her children that got her into drugs.
When her daughter was three, Charlotte was introduced to the idea of selling drugs for extra income. She didn’t do drugs then, never had even tried them except experiments with marijuana when she was younger. Charlotte was a young mother, the only one working in her family, and she was struggling.
She vividly remembers the trouble her own parents had in providing for her and her siblings, and she wanted more. The drugs seemed like an easy – and popular – answer.
So, she got herself a prescription for pain medication and began a lucrative side business in peddling pills. Soon, both she and her husband were doing the drugs, too. Vicodin 10s turned into Percocet 5s. Then the Percocets turned into 15 mg pills. Soon she was taking four a day, with morphine as well. When the 80 milligram OxyContin pills came on the market – known as OC80s – she got hooked and stayed hooked for about a year.
Everyone she hung out with was buying and selling drugs – pills mainly. “It was just there,” she said. “Everyone was doing it.”
She describes herself as a responsible user, she worked, she always put her family first, she kept her kids safe, she kept the income stream coming. She detoxed from the OC80s on her own, and went back to smaller pills. It was manageable, but not what she wanted.
“I woke up one day … looked at my kids …. realized they were being raised in front of a television,” she said. She had to quit.
Her solution? Begin buying the treatment drug Suboxone off the street and self-medicate her way out of the addiction. That didn’t work well, because she didn’t get the doses right.
She was tired of the drug-centered life. “It’s the worst thing. You wake up, and all you can think of is who can I call, where can I get it. It gets so sickening,” she said.
When she was offered a permanent job where she would need to take a drug test, she knew the time had come to quit for real. She became a patient of Northwestern Partners in Hope and Recovery and restarted a clean life that she’s maintained for six years now.
Though not tall in stature, Charlotte always fills a room with her energy. Her words speed out like sparks from a firecracker during her visits at the Partners in Hope and Recovery clinic. Her intensity is softened by an easy smile and an infectious laugh.
Despite her continuing battle with chronic pain related to serious problems with her spine, she has much to be thankful for these days, and she isn’t afraid to share. With grit and determination, she has turned away from drugs to make a healthier life for herself and her family. She shows up consistently to keep herself on track and she has earned her pride in her recovery.
She and her husband stayed together through difficult times, she worked to save for and buy a home of her own on 11 acres. She’s able to provide the life for her son and daughter that she always wanted. “Everything I didn’t get growing up, I give to them,” she said.
Over the last several years Charlotte has demonstrated such consistency with her appointments and urine drug screens that she has progressed to visits only once monthly, says Medical Director Dr. Suzan White. The Suboxone medication she takes not only prevents cravings to return to dangerous use of drugs on the street, but it also helps to take the edge off her chronic pain.
“The stability in her recovery from use of drugs has allowed her to become more stable and fully present in her relationships with her husband and her children. This stability has also provided a foundation for her recent decision to go back to school to prepare for a meaningful career,” says Dr. White
As Charlotte tells her story, she has great insight into how destructive her previous lifestyle was to herself and her family.
Yes, she’s had slip-ups. And no, the life isn’t perfect. At times, she finds the maintenance doses of Suboxone a frustrating process. The regular appointments, the urine tests, the feeling of always having to answer someone … it’s difficult. But it has helped her stay on track, she feels solid, she doesn’t worry. “It’s my safety crutch for now. It’s allowed me to live, to grow, to make better decisions,” she said.
While the recovery journey hasn’t been easy for her, Charlotte credits her success in part to the support team at Northwestern Partners in Hope and Recovery. She and her husband have had financial struggles, and nearly lost their house at one point. But staff at Hope and Recovery pointed her toward a mortgage modification that saved them.
That kind of help with things not directly related to addiction is key to the services at Hope and Recovery, she said. The team there goes far beyond the prescriptions and UAs and becomes a resource community, a different kind of family.
Another example of that wrap-around service is the support and advice Medical Director Dr. Suzan White has given her about her son’s ADHD behaviors. Having someone to talk to who offers helpful support makes a huge difference for Charlotte.
“They take you as a whole package,” she said. That inclusive, non-judgmental treatment helps people ground their recovery in their whole life with all its aspects and impacts. “It’s not just a one-person recovery,” said, Charlotte, “it’s a family recovery.”
She’s now taking classes at the Community College of Vermont and thinking about what her future career might hold. She’s spending time with her kids and husband, and enjoying their simple lives together. She knows first-hand that recovery is the work of a lifetime, but she offers passionate advice to others embarking on their own recovery.
Failure leads to success, she said, encouraging others to be proud of every step they take. “Be proud of the fact that you made the decision,” she said. Recovery takes struggle, heartache, ups, and downs. “But at the end of the day, anything is possible,” she said.
{Y}our Tomorrow
Lauri Ellis

At NMC we know that our future impacts yours. This year we created a campaign that would give us the opportunity to explain our goals, celebrate how we’re growing together, and share new ideas and stories. The {Y}our Tomorrow campaign features stories about what we’re working on to build a healthier tomorrow for our community, testimonials from patients and community members, and a question and answer section where you can get involved in the dialogue with NMC. Check it out oline at: tomorrow.northwesternmedicalcenter.org.
Back in Balance
Linda Pelkey

Highgate – Upon waking one morning, Linda Pelkey was alarmed as she sat upright in bed and immediately fell backwards, unable to keep her balance.
“I can’t tell you how scary it was,” says Pelkey, 55, who had experienced episodes of mild Vertigo in the past. She endured the dizziness all weekend, waiting until Monday to visit the ER at Northwestern Medical Center, where they performed cardiac tests and ruled out the possibility of a stroke.
Most people are familiar with Vertigo, a sudden sensation of dizziness or spinning, often triggered by rapid head movements. Yet, those who have experienced prolonged episodes know just how uncomfortable and disruptive it can be.
“Vertigo has a big impact on what you can and can’t do,” says Pelkey. “It’s not life threatening yet can really limit you.” Though her bouts of nausea were minimal, the dizziness and periods of imbalance that Pelkey suffered would persist for nearly five months.
During those first few weeks, Pelkey met with her Primary Care Physician, Dr. Terri Nielsen, to set a course of action for diagnosis. She underwent an MRI and was also seen by a Chiropractor for possible alignment and gait issues, neither revealing a cause for the dizziness. Pelkey then attended Physical Therapy which provided no relief. She met with a Neurologist at UVM for a series of motor coordination exams, including the Romberg Maneuver.
“It was becoming a long road toward resolution,” Pelkey says about multiple specialist visits, also noting the hefty deductibles. Although she was working hard to be healthy, the Vertigo began impeding her routine. Under the guidance of Dr. Nielsen, Pelkey had stopped smoking three years prior with the help of tobacco cessation counseling.
With rejuvenated lungs, she lost a substantial amount of weight through diet and exercise. Joining New Beginnings in Swanton, Pelkey says it was her first time in a gym, “They really made me feel at home,” even attending an eight-week course on healthier eating. But, when the swaying and nausea began hindering her gym workouts, she had to stop.
Her symptoms were often exacerbated when moving quickly between seated and bent or standing positions. “I began compensating and limiting my movements,” she says, to eliminate triggers. “I was very cautious in the way I would move my head.”
Increasingly frustrated, Pelkey says she was ready to ‘throw in the towel.’ “Yet, I knew it was a physical issue, and that there must be a resolution. Dr. Nielsen encouraged me not to give up,” she says.
It was now July, and Pelkey was referred to Northwestern ENT specialist Dr. Kahren Aydinyan, DO, for audiology exams. Dr. Aydinyan recognized Pelkey’s symptoms as Benign Paroxysmal Positional Vertigo (BPPV), recommending Vestibular Rehabilitation. The function of the vestibular system is to send signals to the brain about head and body movements relative to gravity; with this type of physical therapy being recommended for recurrent vertigo, to help train the other senses to compensate.
A bit weary, as physical therapy hadn’t alleviated her symptoms before, Pelkey met with Anna Krahn, DPT, at Northwestern Orthopaedic and Rehabilitation Center, for a specialized assessment. Utilizing a tool introduced to their practice in October 2018, digitized video goggles called Frenzel Goggles, Krahn was able to capture video recordings of Pelkey’s nystagmus (uncontrolled, rapid eye movements), enabling her to reassess the video for better diagnosis.
“The goggles have a camera that focuses on the pupil of the eye and records the movement. This can be viewed in larger size and slower motion through the computer, which is very helpful because often the symptoms occur very quickly and can be easy to misdiagnose,” says Krahn.
“We also have the capability of putting the patient in the dark, through blacking out the lens of the goggles,” she says, which still records the eye’s movement. “This is very helpful for diagnosing individuals who have learned to stabilize their eye movements by focusing on objects in the room,” as Pelkey had learned to do.
“In Linda’s case, it seems that the therapist who had seen her prior may have misdiagnosed the nature of her nystagmus, thinking that the problem was in a different area of her vestibular system,” says Krahn. “Her nystagmus occurred very quickly and would have been easily missed if we had not been able to review the testing with the video captured by the goggles.”
The diagnosis was indeed BPPV, affecting Pelkey’s left side. With the assistance of another therapist, Krahn moved Pelkey’s head in a series of positions (Canalith Repositioning Maneuver) to try and get the inner ear crystals, called otoconia, to move back to their correct location.
“The head positions vary, depending on where the crystals are out of place. It takes the skill of the physical therapist to determine which area of the inner ear is impacted as the treatment position is specific to an individual’s presentation,” she says.
“I could tell the difference right away,” says Pelkey, relieved. “Anna had fixed it!” She then asked Krahn what she could do to prevent it from happening again.
“BPPV typically occurs for no known reason. You are more likely to get it again if you have experienced it before,” says Krahn. “While BPPV is the most common diagnosis for individuals with episodic vertigo, it’s also the type that responds most quickly to Physical Therapy treatments.”
BPPV typically affects individuals who are over the age of 45 years, with women more likely to be affected then men. NMC’s therapists say they regularly see patients dealing with vertigo, sometimes two or three a day. “The good news is many patients only need to be seen for one visit and their symptoms resolve, others may have to be seen a few times.”
With the aid of the Frenzel Goggles, such delays in diagnosis and treatment, should be a thing of the past. “Frenzel Goggles are the cat’s meow, without them I’d still be struggling,” says Pelkey.
“The goggles have allowed us to improve our accuracy with diagnosing the specific cause of a patient’s vertigo, particularly for patients who have BPPV. They have been a great educational tool for our patients so they can better understand the testing process and what we are watching for,” Krahn says.
“We are hoping to learn even more ways that we can utilize these goggles in the future, that may be able to assist us with treating individuals with symptoms of vertigo, as well as concussion.”
For anyone dealing with vertigo symptoms, NMC’s physical therapists recommend avoiding activities that make your symptoms worse, such as sudden head movements. They suggest talking with your doctor to ensure there are no other medical issues contributing to your dizziness; and asking for a referral to see a physical therapist who can evaluate and treat vertigo.
“When you know something is wrong and it’s not your natural state you must continue until you have the answer. Keep on the path until you find the right person who will diagnose you and fix the problem,” Pelkey offers, to others who might be struggling.
“In the end, all of the tests were beneficial. I got my eyes and ears checked. I’d never had my hearing tested before, and at my age it was good to have it done,” says Pelkey.
“I was close to just accepting the limitations that my body was encountering. It brings you down mentally; the frustration, anger, and pattern of emotions when you don’t have answers.”
Pelkey is now playing catch-up, finishing all the projects she couldn’t tend to this summer, with plans to get back into the gym. “Once I was fixed, I got my life back,” she says, “I got myself back.”
Meeting Community Needs
New Providers
NMC has a bumper crop of new providers joining our staff this fall, in the fields of Primary Care, Orthopaedics, Pediatrics and Obstetrics and Gynecology.

Dr. Elizabeth Disney
Northwestern OB/GYN
About Dr. Disney
Dr. Elizabeth Disney started practice with Northwestern OB/GYN in August. She is originally from Plattsburgh, NY and recently completed her four-year OBGYN residency at the University of Utah Hospital in Salt Lake City. She said she enjoys caring for women of all ages, through their greatest triumphs and their most challenging hardships. She spends most of her free time in the outdoors, trail running, skiing and playing on the lake.

Dr. Nathan Mauser
NW Orthopaedic and Rehabilitation Center
About Dr. Mauser
Dr. Nathan Mauser began work with the Northwestern Orthopaedic and Rehabilitation Center in mid-September. Dr. Mauser earned his medical degree from the University of Louisville School of Medicine and performed his residency at the University of Vermont Department of Orthopaedics and Rehabilitation. He also did a spine fellowship at the University of Pittsburgh Medical Center Department of Orthopaedics. He has strong family ties to the area and said that “Vermont and NMC are the perfect blend of natural beauty and community. I have always wanted to work at a community hospital. NMC has allowed me to create a practice specializing in my two favorite areas of orthopaedics: total joint replacements and spine surgery.”

Dr. Cecilia Disney
Primary Care provider
About Dr. Disney
Dr. Cecilia Disney, also joined NMC this fall! Dr. Cecilia Disney is a Primary Care provider and joins the teams at Northwestern Primary Care in St. Albans and Northwestern Georgia Health Center. Cecilia is excited to join her sister Elizabeth on NMC staff, but said that it was really the people and staff at Northwestern Medical Center who helped her make the decision to come to Vermont from the Sea Mar Community Health Centers near Seattle where she had been practicing. “You have to be energized by your colleagues,” she said, something she experienced during her interview process. Dr. Disney also said she enjoys family practice because it allows her to get to know people deeply, and to connect with whole families.

Dr. Colleen Moran
Northwestern Pediatrics
About Dr. Moran
Dr. Colleen Moran also started at NMC this fall, joining the team at Northwestern Pediatrics. Dr. Moran is a Vermont native who earned her MD from the UVM College of Medicine, and performed her residency at the UVM Children’s Hospital. She enjoys working with kids and families at all stages of growth and development. In particular, she enjoys caring for adolescents as they transitioning into early adulthood. “Adolescence is a time of incredible change and growth,” says Dr. Moran, “and I like to work with patients and families to support the natural transition to independent young adulthood.”
Dr. Moran is delighted to be settled in Vermont with her family and pets, including horses.
Additional new Providers:
- Kaitlyn Barrett, DO, Endocrinologist
- Christine Corbeil, NP, Cardiology
- Ludmila Kaplan, MD, Hospitalist
- Lucy Lane, MD, Radiologist
- Blake McKnight, NP, Urgent Care
- Elizabeth Owens, PA, Urgent Care
- Lauren Pelski, NP, Urgent Care
- Meghan Saunders, NP, Hospitalist
- Mary Alice Watts, NP, Primary Care
- Robert Yeager, MD, Emergency Med
Coming Soon:
- Shannon Hogan, DO, Pediatrician (starting 11/18)
- Andrew Myrtue, MD, Orthopaedics (starting 3/2020)
- Shaunna St. Clair, PA, Urgent Care (starting 2/2020)
Community Events
Pediatrics in Action
Dr. Laura Bellstrom got in on the fun at Healthy Hearts as part of the Northwestern Pediatrics booth that encouraged kids to be physically active through things like hula hooping.
Bashaw Bowlathon
This year’s Bowl-a-Thon to support the Jim Bashaw Cancer and Catastrophic Illness Fund raised over $7,200 thanks to generous sponsors and dedicated bowlers. The annual event is one of the biggest fund-raisers for this worthy cause.
Fun with Flavorland
Health Educator Amy Brewer plays Flavorland with a young attendee at the Healthy Hearts event held at St. Albans City School. The event drew hundreds of families for a half-day of healthy fun and education.
Learning About Stress Reduction
NMC’s Deb Timmerman is a Senior Pharmacy Technician at NMC, and she volunteered at the Family Birth Center booth at Healthy Hearts. This year, the FBC encouraged people to engage in mindful activities like knitting, crocheting or making friendship bracelets. This kind of mindful behavior can help calm parents and children!
Connecting with the Community
Shannon Meehan, Exercise Physiologist, plays Healthy Jeopardy with a Healthy Hearts attendee. Meehan’s booth included fun facts from NMC’s Cardiac Rehab and Pulmonary Rehab programs – teaching about hearts and lungs.
Volunteerism
at NMC
NMC Connecting to Community
This year, NMC staff began two programs of regular community service – helping the local food shelf and soup kitchen.
This year, NMC collaborated with other community organizations to help Northwest Family Foods stay open one evening each week – giving access to the food shelf during after-work hours. One Thursday evening each month, NMC’ers volunteer at the food shelf to help the Northwest Family Foods staff extend the hours of service. The Franklin County Business and Professional Women and the St. Albans Rotary Club join NMC in the week-night volunteering – a true community collaboration.
In another volunteer activity, NMC Departments volunteer each month to gather staples for Martha’s Community Kitchen, supporting the organization’s work in providing lunches for community members every day from 11 am to 12:30 pm. Staff provide needed items like spaghetti, beans, coffee, iced tea, sugar, cleaning products, responding to need expressed by Kitchen staff. Martha’s Kitchen has been a part of our community for 30 years, and this year moved to a new location on Lake Street.
Bill Young is a Switchboard Operator at NMC and part of the Patient Access team who collected staples for Martha’s Kitchen this year.
Members of NMC’s Laboratory Services team donated this collection of food staples for Martha’s Kitchen.
Darcy Tatro and Suzette Gagne of NMC’s Finance Department spent an evening volunteering at Northwest Family Foods this year, helping stock and organize shelves.
Investing for a Healthier Community
As a not-for-profit organization and as one of the largest employers in the region, NMC carries a responsibility, both formal and informal, to help address critical issues which impact community health that go beyond the direct care NMC provides. We do so through our ‘community benefit investments’ (a term of the Internal Revenue Service – IRS) to help our community achieve a healthier future.
Northwestern Medical Center receives financial benefits by participating in the 340B drug pricing program. These benefits contribute to the level of financial assistance that NMC can make available to patients who meet established criteria. No specific discount or financial assistance is offered to patients that receive drugs under the 340B drug pricing program; however, these patients can apply for NMC financial assistance that is available to all who qualify.
Lack of financial resources is a barrier to good health. To help, NMC provides free care for those who meet guidelines (income below 300% of the poverty line). That amounted to close to $1 million of free care in Fiscal Year 2018. We also contribute to and administer the Jim Bashaw Cancer and Catastrophic Illness fund, the NMC Diabetes fund, and the Smiles for Recovery fund which assist patients with healthcare expenses. In addition, NMC provides flexible funding through our care management process to help patients address social determinants that interfere with their recovery and good health.
NMC’s vision calls on us to “partner to improve the wellness of our community.” Investing in wellness and prevention to prevent illness and chronic disease and reduce the demand for costly medical treatments is a vital part of bending the cost curve in healthcare long term and improving the quality of life. Toward this end, NMC invests more than $1 million in unreimbursed Lifestyle Medicine Services, the RiseVT community campaign to embrace healthier lifestyles, community care management, and related services and offerings. NMC partners with Northwestern Counseling & Support Services to bring the “Healthy Hearts” health fair to the community each February, providing access to education, free screenings, referrals, and family fun for hundreds of attendees. We are a significant funder for the Franklin Grand Isle Tobacco Coalition efforts, which has been instrumental in reducing the rates of tobacco use in our community. We are the major funder of the Healthy Roots Collaborative, the diversified agricultural effort in our local region which is helping fresh healthy local produce and foods into homes across our community.
We are also a significant financial partner in the Congress & Main development in partnership with Vermont Tech, Community College of Vermont, and the City of St. Albans to expand a nursing program into downtown infused with wellness services. The return on these investments is long-term and it is real. The national Prevention Institute says, “For every dollar we spend on prevention we see a 5 to 1 return on investment in just 5 years. We simply can’t fix our economy without it.”
On top of these focal efforts relating to community benefit, NMC provides close to $100,000 a year in funding to key community partners working on priorities within the community health needs assessment, on social determinants such as housing, and on related efforts to improve the quality of life. These agencies are able to have a positive impact in areas outside NMC’s direct expertise, but which directly impact the lives of our patients and our staff. NMC is a significant funder of the United Way of Northwestern Vermont and also provides donations and support to partners including: the American Heart, Cancer, and Alzheimer’s societies; Martha’s Kitchen; Tim’s House; Franklin County Home Health; Hard’Ack; the Franklin County Regional Chamber of Commerce; the Vermont Futures Project; the Howard Center; Special Olympics; Make A Wish; Northwest Family Foods of CVOEO; Mobius Mentoring; the Teen Institute; Voices Against Violence; Girls On the Run; the Friends of Northern Lake Champlain; Prevent Child Abuse Vermont; the St. Albans Rotary Club; and more. In addition, this year, NMC employees have joined in on the effort to serve our community, with an initial focus on helping local efforts to address food insecurity. In a partnership with Northwest Family Foods, NMCers are among the volunteers working to keep the food shelf open one evening a week. This allows individuals and families who need access but who are working full time to be able to come to the food shelf after work. NMC staff are also taking turns once a month with departmental food drives to provide meals and needed supplies to Martha’s Kitchen. Monthly donations can weigh in at more than 90 pounds and make a valuable difference to our partners’ efforts to provide meals for those in need. No single individual or agency can tackle the challenges of our community alone and NMC is proud to collaborate with these great partners as we work collectively towards a healthier future for all.
New Ventures
Name Change: Northwestern Partners in Hope and Recovery
This year, Northwestern Medical Center “pain clinic” adopted a new identity that better reflects the mission and approach of the clinic: Northwestern Partners in Hope and Recovery. This new name gives clearer representation of the work of the team which partners with community members who are working to overcome addiction. The butterfly in the logo is unique among the NMC practices, and represents the transformative changes many of our patients make in the process of recovery and growth.
“With expanded services including educational groups, psychiatry, medication management, multiple care providers, nursing care coordination, mindfulness and social work, we are well equipped to provide a whole-person, holistic approach to recovery,” says Medical Director Suzan White.
“It is our goal to create a foundation for lasting change in individuals who are ready to move toward a more stable and healthy life. Our experienced team facilitates this transformation by treating everyone who walks through our doors with kindness, caring and respect,” she says.
New Services, Greater Access
NMC continually strives to meet community need for healthcare and this year, we launched several new services, and partnered with other healthcare organizations to strengthen the local care system.
In the fall of 2018, Northwestern Occupational Health began providing telemedicine visits for injured worker care for two Vermont businesses, saving time and travel for their employees
The two St. Albans offices of the Northern Tier Centers for Health moved onto NMC’s campus in March 2019, offering patients convenient parking and quick access to hospital services as well from their location in Suite 3 of the Doctors Office Commons building.
In April, NMC announced a partnership with Vermont Tech and Community College of Vermont to bring a nursing program and wellness resources to downtown St. Albans in the building project at the corner of Congress and Main Streets. This collaboration anchors health, wellness and education right at the heart of our community, a big win for the local economy, for the business community, for local students and for the healthcare field so urgently in need of qualified nurses.
NMC launched its Hearing Aid Clinic in the spring, bringing much-needed access to area residents seeking help with hearing aid assessments, purchase and fittings.
On July 1, NMC’s infusion medicine services moved into a new location – the West Wing of the Progressive Care inpatient unit. The location provides dedicated space for infusions, moving out of shared space in the operating suites.
In the fall of 2019, NMC began offering endocrinology services in partnership with the University of Vermont Medical Center, using a UVVMC physician two days per week in NMC’s specialty clinics space at the front of campus.
Coaching a Village to Health
One key focus for NMC’s Lifestyle Medicine Clinic this year is a Health Coaching approach – a technique that involves a triad of providers: Physician, Dietician and Athletic Trainer. The Health Coaching model is all about building relationships, says Athletic Trainer John Burke. That relationship enables a Health Coach to uncover a patient’s motivators … and finding those intrinsic reward systems leads to sustainable changes.
“It also gives patients a platform to be heard,” says Burke. “When was the last time they were truly and deeply listened to?”
A Health Coach is there to listen, and to reflect what patients say, responding with empathy and compassion. That listening session starts the whole process of creating a wellness vision, setting short and long-term goals, and looking to the future.
“This behavior change mindset is key to making changes in your lifestyle that you will be able to maintain over time,” says Lifestyle Medicine Medical Director Elisabeth Fontaine, MD
And, when individual efforts like Health Coaching meet up with community-based changes – like those supported by RiseVT – successful wellness is much easier to achieve and sustain.
Want to meet with a Health Coach?
Call 524-1227 to make an appointment today!
Investing in Prevention
Feet on the Ground: Getting Active with Walkability Expert Mark Fenton
Walkability expert Mark Fenton visited the towns of Alburgh, Enosburg Falls, Fairfax, Grand Isle, Highgate, Montgomery, Sheldon, St. Albans and Swanton this spring, as part of collaborative efforts to make local communities more walkable and more bikeable. Fenton was making a repeat visit to our area, having toured here in 2015, and he both reviewed progress made and recommended continued improvements.
The visit was made possible by RiseVT with planning help from the Northwestern Regional Planning Commission and the Vermont Department of Health. Fenton’s visit was inspiring, as he spoke with many community members throughout his visit, applauding their efforts and urging them to keep the momentum going.
His key message: design your communities to encourage physical activity – specifically walking. These design and infrastructure changes will be good for individual health, will attract new homeowners, and strengthen the local economy.
One of the remarkable elements of his visit was the deep engagement in each town he visited. He was met with community leaders, business people and citizens who were excited to share and learn – and he encouraged them to be unafraid to try small changes, temporary measures and pilot projects to get the walkability ball rolling.
He was impressed with work in Swanton where the community implemented many improvements since the 2015 visit. He emphasized that community change takes community partnerships and thanked RiseVT for providing impetus and support for such change. “If you don’t have good community partners like {RiseVT} to work with, nothing gets done,” he said.
Mark Fenton and a group of Fairfax residents cross the covered bridge near the elementary and high school on Maple Street.
Touring the St. Albans Bay area, Fenton took note of the dangerous intersection of Lake Street and Georgia Shore Road, recommending curb extensions, high-visibility crosswalks and curb bump-outs.
Fenton visited Highgate, walking the Health Path with Heidi Britch-Valenta in this photo.

In Montgomery, Fenton visited with community leaders, staff and residents. He recommended the town adopt a “complete streets” policy that ensures that all road work takes all users into account, including pedestrians and bicyclists.
Prevention Ride with the Governor
In August, Governor Phil Scott toured Franklin County on his bike with a group of local cyclists taking a journey designed by RiseVT to promote wellness, primary prevention of chronic disease, and build on the rolling momentum of a visit by national walkability expert Mark Fenton.
The Governor embarked on the trip from Northwestern Medical Center, and from there headed to the St. Albans Bay Park. He was met by RiseVT Wellness Specialist Jessica Frost, who introduced Town Select board Chair Brendan Deso and Melinda White of NMC’s Northwestern Partners in Hope and Recovery. Both Deso and White spoke of the importance of walkable communities – which support businesses, quality of life, and even recovery.
Next the Governor’s riding group headed to Swanton where they celebrated 10 years of the Swanton Fit and Healthy Path and visited a new playground. The crowd in Swanton was strong, demonstrating that community’s engagement on healthy programming and infrastructure.
From Swanton, the group rode to Highgate, once again met by a crowd of community members and officials who showed off the area’s work on walkability.
The event was a successful showcase of the concepts behind thoughtful design of the built environment. This thoughtful approach has big impacts on creating safe, walkable, bikeable environments for all. This kind of environment fosters health and wellbeing through physical activity and community connectedness.
New Wellness Policy for Maple Run
This June, the Maple Run Unified School District adopted a new wellness policy aimed at creating healthier school environments and ultimately reducing childhood obesity.
The new policy was developed collaboratively with input from many groups, and with support from RiseVT. A group of advocates came together with about 20 active members that included nurses, guidance counselors, teachers, Vermont Department of Health staff, parents, physical therapists, Farm to School experts, The Abbey Group and staff of the school district office. This group met regularly for nearly two years to evaluate the existing policy, and craft a new one.
The group used a Wellness School Assessment Tool (WELLSAT) and found that the old policy scored a 33/100. RiseVT also conducted a measurement study of BMI averages for the school district. The results showed obesity rates as high as 28 percent in one of the Maple Run school districts. These numbers prompted school officials to take action.
The new policy has schools building physical activity into classroom activity, implementing Farm to School programs, using healthy foods in celebrations, adopting “share fridges” to address hunger and eliminate waste … and much more. The collaborative process and widespread impact of the policy change make this milestone a major marker on our area’s journey to health.
RiseVT encourages stretch breaks for kids in classrooms.
St. Albans City School students take part in a wall sit challenge.
RiseVT is Rising to the Occasion
Many local schools, businesses and municipalities have risen to the challenge set by RiseVT to actively create healthy environments. Schools tap into the energy of staff and students, businesses build flexible, innovative wellness programs for healthy workplaces, and cities and towns commit to policy changes that support healthy community environments. This great work locally has inspired the RiseVT movement to grow statewide. Click here to learn more about the statewide effort.
Here’s a list of the rising tide of healthy heroes!
Gold Schools
View Gold Schools
- Bakersfield Elementary Middle School
- Fairfield Center School
- Fletcher Elementary School
- Georgia Elementary and Middle School
- Sheldon Elementary School
- SOAR Learning Center
- St. Albans City School
- St. Albans Town Educational Center
Thank you to the dedicated classroom teachers who have made this gold-level success possible!
Gold Businesses
View Gold Businesses
- Ben & Jerry’s
- Community College of Vermont
- City of St. Albans
- Duke’s Fitness Center
- Franklin County Caring Communities
- Franklin County Home Health Agency
- Franklin Northwest Supervisory Union
- Maple Run Unified School District
- Northwestern Counseling & Support Services
- Northwestern Medical Center
- The St. Albans Museum
- Swanton Village
- Vermont Department of Health
- Vermont Precision Tools
Gold Municipalities
View Gold Municipalities
-
City of St. Albans
-
Swanton Village
-
Town of Highgate
-
Town of St. Albans
RiseVT Gold Level Teachers
Kendra Pillsbury
Bakerfield Elementary Middle School
Meghan Petrie
Bakerfield Elementary Middle School
Arlene O’Rourke
Bakerfield Elementary Middle School
Cara Newman
Bakerfield Elementary Middle School
Kiah Hamner
Bakerfield Elementary Middle School
Chelsea Ellis
Bakerfield Elementary Middle School
Stephanie Beland
Bakerfield Elementary Middle School
Madison Sanguinetti
Fairfield Center School
Kathleen Pellegrino
Fletcher Elementary School
Cathy O’Brien
Fletcher Elementary School
Alison Perry
Folsom Education and Community Center
Samantha Cantell
Folsom Education and Community Center
Erin Young
Georgia Elementary and Middle School
Sue Tougas
Georgia Elementary and Middle School
Stacey Sullivan
Georgia Elementary and Middle School
Heather Sikorsky
Georgia Elementary and Middle School
Emily Morse
Georgia Elementary and Middle School
Allison MacKenzie
Georgia Elementary and Middle School
Jessica Howrigan
Georgia Elementary and Middle School
Sara Heth
Georgia Elementary and Middle School
Pam Farmer
Georgia Elementary and Middle School
Mandy Alarcon
Georgia Elementary and Middle School
Robin Taylor
Grand Isle School
Kathleen Williams
St. Albans City School
Michelle Patnode
St. Albans City School – now teaching in Highgate
Kristen Murphy
St. Albans City School
Lauren Mangis
St. Albans City School
Lisa Lucas
St. Albans City School
Sally Lawyer
St. Albans City School
Tiffany Johnson
St. Albans City School
Tyler Cook
St. Albans City School
Braina Brown
St. Albans City School
Anna Brace
St. Albans City School
Jessica Bachand
St. Albans City School
Amy Ward
SATEC
Lisa Thompson
SATEC
Kate Pelkey
SATEC
Dina Fitzgerald
SATEC
Cheryl Duplissa
SATEC
Daphne Delude
SATEC
Lisa Curry
SATEC
Jennifer Callahan
SATEC
Diane Bruley
SATEC
Jill Boomhover
SATEC
Regan Keelty
Sheldon Elementary
Kerri Hoag
Sheldon Elementary
Sarah Farrar
Sheldon Elementary
Kelly Derry
Sheldon Elementary
Lisa Cioffi
Sheldon Elementary
Amy Callan-Gervais
Sheldon Elementary
Jessica Bourbeau
Sheldon Elementary
Heather Young
SOAR
Tiffany Trombley
SOAR
Randy Pike
SOAR
Kristi Hamblett
SOAR
Caitlin Farrar
SOAR
Matt Chevalier
SOAR
Marc Brunelle
SOAR
Hannah Scott
Swanton Elementary School
Gabby Ramseyer
Swanton Elementary School
Jamie McCarthy
Swanton Elementary School – now teaching in Essex
Jody Chase
Swanton Elementary School
Braina Brown
SACS
Braina Brown
SACS
Anna Brace
SACS
Jill Boomhover
SATEC
Tess Bashaw
SACS
Jessica Bachand
SACS
Our People
Clinical Practice Governance Milestones
This year, NMC made a tremendous amount of progress implementing a new Clinical Practice Governance model. This shared-decision making structure is related to the clinical care of patients, family and community served by NMC. The CPG model includes Unit-Based Councils representing distinct clinical departments to discuss, investigate and develop plans on healthcare practice. The model also includes a Coordinating Council to support interdepartmental communication about policy and procedure to ensure consistency and collaboration.
February
2.15.19
Shared Governance Advisory Group Retreat
March
3.12.19
Shared Governance Advisory Group regular meetings began
More than 30 nurses gathered for the Clinical Practice Governance day-long retreat held in September.
April
4.10.19
Logo, FAQs, Nomination Process, and Roles & Descriptions documents developed & finalized
4.19.19
Vicki George, PhD, RN, FAAN visited for the CPG Kickoff
4.22.19
Nurses nominate members of their departments they’d like to be members of the CPG Unit-Based Council
June
6.13.19
Nominees notified
6.25.19
Nominees to submit “Get to Know Me” forms by this date if interested in participating in the CPG Unit-Based Council
July
7.08.19 to 7.22.2019
Voting period
7.11.19
Adirondack Health visits to discuss their “Shared Governance Journey”
Working session
Nurses who were elected to the Unit-Based Council as well as the Coordinating Council gathered in September for a planning retreat led by consultant Vicki George, PhD, RN, FAAN.
August
8.20.19
Announce CPG Members
SEPTEMBER
9.06.2019
Transition to Practice Governance Retreat – Vicki George, PhD, RN, FAAN
Highlights of Happenings
Governor’s Visit During Nurses Week:
Governor Phil Scott visited NMC during our annual Nurses Week Celebrations and signed a proclamation formally recognizing the day in honor of nurses. He’s pictured here with some of NMC’s nursing staff and nursing leadership at a welcoming event held in the Courtyard Café.
Service Excellence Award Winner
Linda Martell, MA (center) was honored with the Service Excellence All-Star of the Year Award at June’s Employee Service Awards Recognition Banquet. Linda was recognized as someone who genuinely cares about her patients, her co-workers and her peers and was described as professional, respectful, resourceful and kind.
Pedal Powered Maple Fest Float
This year, NMC debuted a surrey bike at the Maple Festival Parade to show that embracing healthy lifestyles is not only important – but fun as well! Both RiseVT and NMC staff teamed up for the pedal-powered parade entry.
Celebrating Hospital Week
Chief Nursing Officer Deanna Orfanidis, RN serves up lunch during the Hospital Week free staff luncheon. Each year in May, NMC celebrates all staff with a week of fun, games and prizes – a staff favorite is the amazing free meal prepared by our Restaurant and Catering team and served by Leadership and Management.
Staff Feature
Nurses Making a Difference

Karen Fitzgerald and Leah Jablonski, both nurses in NMC’s Family Birth Center, made a missionary trip to Haiti this January – an experience that changed their perspectives on life in America.
The two spent 12 days in Haiti, working with an organization called Friar Suppliers, which makes regular trips to Haiti to support the local communities with supplies, food, water, jobs, and housing. During their trip, Karen and Leah helped to distribute food and clothing and also worked in the medical clinic.
Both remarked on the joyful, welcoming openness of the Haitian people, despite their lack of what we would consider basic necessities – water, food, clothing, medical care.
“It’s moving to me to this day,” said Karen. “It comes into my mind almost every day.”
Leah agreed. “It makes you do some self-reflection, this is why it’s so powerful.” She described the Haitians she met as beautiful, vibrant people in a culture very different from our own. “They go for days or weeks without water. And yet, they’re happy.”
Karen has supported the Friars Suppliers organization through donations for about 8 years and had gone on one previous Haiti Mission. But this year’s trip was a new experience for Leah – and she brought her husband along as a kind of honeymoon, the couple having married recently.
For both nurses, the experience was life-changing. They came back to view pantry cupboards as a wonder, and to marvel at the luxury of a long, hot shower.
For several days of the trip, Leah helped sort donated goods for pickup by Haitians and Karen helped teams building houses – 10×12 plywood sheds with one door and one window. Then, the two nurses helped staff the medical clinic.
During clinic hours, Leah’s role was to take manual blood pressures and it was typical to take a minimum of 200 BPs per day – all performed in extremely hot temperatures. The Haitians waited patiently in orderly lines for hours in the heat, with no complaints. Karen did triage at the clinic and said they saw many patients with stomach complaints that were often the result of parasites, as well as coughs, sore back, sore knees, itchy eyes.
“Some of the people who came through the clinic would break your heart,” said Karen.
But it was the kind and joyful nature of the people, and their deep sense of community that struck both women and remains in their minds. The experience sticks with them, a reminder of the things that are truly necessary for a happy life.
Awards and Honors

Honoring Community Service
Long-time Franklin County Legislator and Registered Nurse in NMC’s Emergency Department Kathy Keenan was honored with this year’s NMC Community Service award.
NMC Board President Leon Berthiaume announced the award on behalf of the board, and honored Keenan for her advocacy for the people of Franklin County both in Montpelier and locally.
“Kathy has been an active force working for the greater good in our community for many years while overcoming challenges and building positive relationships,” said Berthaiume.
“During her service in the Vermont Legislature, Kathy was known as a strong advocate for the people of Franklin County while being attentive to the needs of the state and the means of the taxpayers. She welcomed differing viewpoints and patiently and skillfully moderated many local Legislative Breakfasts to help give constituents an opportunity to share their perspectives and ask their questions,” he said.
Berthiaume also noted her local involvement, serving on board of the Samaritan House, Franklin County Home Health Agency; the NMC Incorporators; the Business & Professional Women’s group; the St. Albans PTO; and the United Way of Franklin County.
Keenan also served as an Emergency Department nurse for more than 20 years. She was active in teaching the ENCARE drunk-driving prevention courses to local youth and helped establish the awareness-raising “THINK” signs which appear throughout Vermont marking the locations of fatalities that occurred as the result of drinking and driving.

DEO Award
Dr. John Minadeo, and Emergency Department Physician and NMC’s new Chief Medical Officer, was honored with this year’s Deogracias “Deo” P. Esguerra, MD Service Award.
The award was created in 2011 to honor a provider with a “passion for excellence and dedication to the patients of our community.” Its namesake, Dr. Esguerra, was known as a caring, passionate and inspirational physician who loved both the science and art of medicine.
At the event where the award was presented, Dr. Minadeo was described as followed in Dr. Esguerra’s footsteps with a strong foundation in patient care, providing the best even under difficult circumstances.
The Men of NMC Tackle Health Topics
June was Men’s Health Month and this year, NMC raised awareness by seeking words of wisdom, tips and tricks from male staff around the hospital. Here is a sample of what they had to say to their colleagues and co-workers.
Click the arrows to see more
Board of Directors
President
Leon Berthiaume, of Swanton. Mr Berthiaume is the CEO of the St. Albans Cooperative Creamery.
Vice President
Janet McCarthy, of Georgia. Mrs. McCarthy is the Executive Director of the Franklin County Home Health Agency.
President of the Medical Staff
Katie Montagne, MD. Dr. Montagne is an Anesthesiologist.
Treasurer
Dawn Bugbee, of South Hero. Mrs. Bugbee is a Vice President and the Chief Financial Officer of Green Mountain Power Corporation.
Secretary
Jake Holzscheiter, of Westford, Mr. Holzscheiter is the President CEO of A.N. Deringer, Inc.
Past President
Kevin Manahan, of St. Albans. Mr. Manahan is a CPA with A.M. Peisch & Company, LLP.
Lorne Babb, MD, of Enosburg. Dr. Babb is a private practice physician and owner of Cold Hollow Family Practice in Enosburg Falls.
John Casavant, of St. Albans. Mr. Casavant is a Risk Management and Insurance professional with NFP.
Nick Hadden, of Fairfax. Mr. Hadden is an attorney.
William O’Connor, Jr, of St. Albans. Mr. O’Connor is retired from the Food Science Corporation where he served as Chief Operating Officer.
Karyn Rocheleau, of St. Albans. Ms. Rocheleau is retired and is a former owner of a Training & Consulting Company.
Marietta Scholten, MD, of St. Albans. Dr. Scholten is a practicing family medicine physician, former Medical Director for the Vermont Chronic Care Initiative and the Medical Director of the Franklin County Hospice Program.
Medical Executive Committee
Kathryn Montagne, MD, President of the Medical Staff
Donny Khela, MD, Vice President
Jennifer Eaton, MD, Secretary
Thomas Harrison, Immediate Past President
Louis Dandurand, MD, Chief of Emergency Service
Michele Burke, MD, Chief of Inpatient Service
David Groening, DPM, Chief of Surgical Service
Terri Nielsen, MD, Chief of Outpatient Medicine Service
Jennifer Covino, MD, Chief of Pediatric Service
Michael Barnum, MD, Member at Large
Leadership Team
Jill Berry Bowen, Chief Executive Officer
Robyn Alvis, Chief Financial Officer
Deanna Orfanidis, Vice President, Chief Nursing Officer
Joel Benware, Chief Operating Officer, Chief Compliance Officer
Jonathan Billings, Vice President, Community Relations
Tom Conley, Vice President, Human Resources & Organizational Development
Amy Putnam, Vice President, Physician Services
John Minadeo, MD, Chief Medical / Quality Officer
Board of Incorporators
Judy Ashley
Lorne Babb, M.D.
Michael Barnum, M.D.
Mary Bates
Reginald Beliveau
Leon Berthiaume
Robert Bessette
George Bilodeau
Bernie Boudreau
Steven Broer, Psy,D
Gregory Brophey, M.D.
Jacqueline Brosseau-Cyr
Lawrence Bruce
Dawn Bugbee
Peter Burke, M.D.
John Casavant
Jane Catton
Sandra Chagnon
David Charbonneau
Paul Clark
Donald Collins
Vaughn Comeau
Coleen Condon-Kohaut
Michael Corrigan, M.D.
David Debellis
Dustin Degree
Christopher Dermody
Lynn Desautels
Richard Dickinson,, D.M.D.
Grace Dickinson-Branon, D.M.D.
Catherine Dimitruk
Hibbard Doe
David Ducham
John Edwards
Nancy Fiske
Elaina Fontes
Bradley Gabree
Steven Gagner
Andrea Gagner
Thomas Gallagher
Elizabeth Gamache
Peter Garceau
Valdemar and Bridget Garibay
Thomas Gates
Clement Gervais
Uwe Goehlert, M.D.
Nilda Gonnella-French
Winton Goodrich
Leon Graves
Monica Greene
William Greenwood
Molly Grismore, R.N.
Nicholas Hadden, Esq.
Joe Halko
Christina Hamel
Warren Hamm, Jr.
John and Lisa Hango
Rett Heald
Gerald Herrera
Hector Hill
Jacob Holzscheiter
Brian Honsinger
Jacqui Hood
Bridget Howrigan Rivet
Shirley Jacobs
Hayden Janes
Celeste Kane-Stebbins
Kathleen Keenan
Ned Kirsch
Dana Kittell
Molly Lambert
Kathy Lavoie
Michelle Lawrence
Chelsey Lawyer
Jeffrey Levesque
Sally Lindberg
Danielle Lindley-Mitchell
Carol Livingston, R.N.
Deborah Loughlin
Adam Luneau
David Mahoney
Kevin Manahan
JoAnn Manahan
James Manahan II
Steven Marshall, Esq.
Sandy Mayotte
Janet McCarthy
Mike McCarthy
Ralph McNall
John Minadeo, M.D.
Sheri Moore
Jeffrey Moreau
Dr. Joseph and Judy Nasca
William Nihan
William O’Connor, Jr.
Corey Parent
Pamela Parsons
Steve Payne, M.D.
Peter Perley
Albert and Marcia Perry
Susie Posner Jones
Kristin Prior
William Roberts, M.D., PhD.
Donna Roby
Karyn Rocheleau
Samuel Ruggiano
Chip Sawyer
Kevin and Karen Scheffler
Marietta Scholten,M.D.
John Schreindorfer
Kristina Senna
Albert and Sally Severy
Heather Skilling,V.M.D.
Tim Smith
Stephen Stata
Molly Stata Comeau
Kathy Tabor
Patrick Talcott
Barbara Toof
Thomas Traber
Paula Tremblay
Ted Tyler, III
Lynn Vallee
Howard Van Benthuysen
Daniel Vanslette
Albin Voegele
James Walsh
Homer Wetherby
Deb Winters
Penny Wright
Frank and Judy Zsoldos
Finance
Financial Report
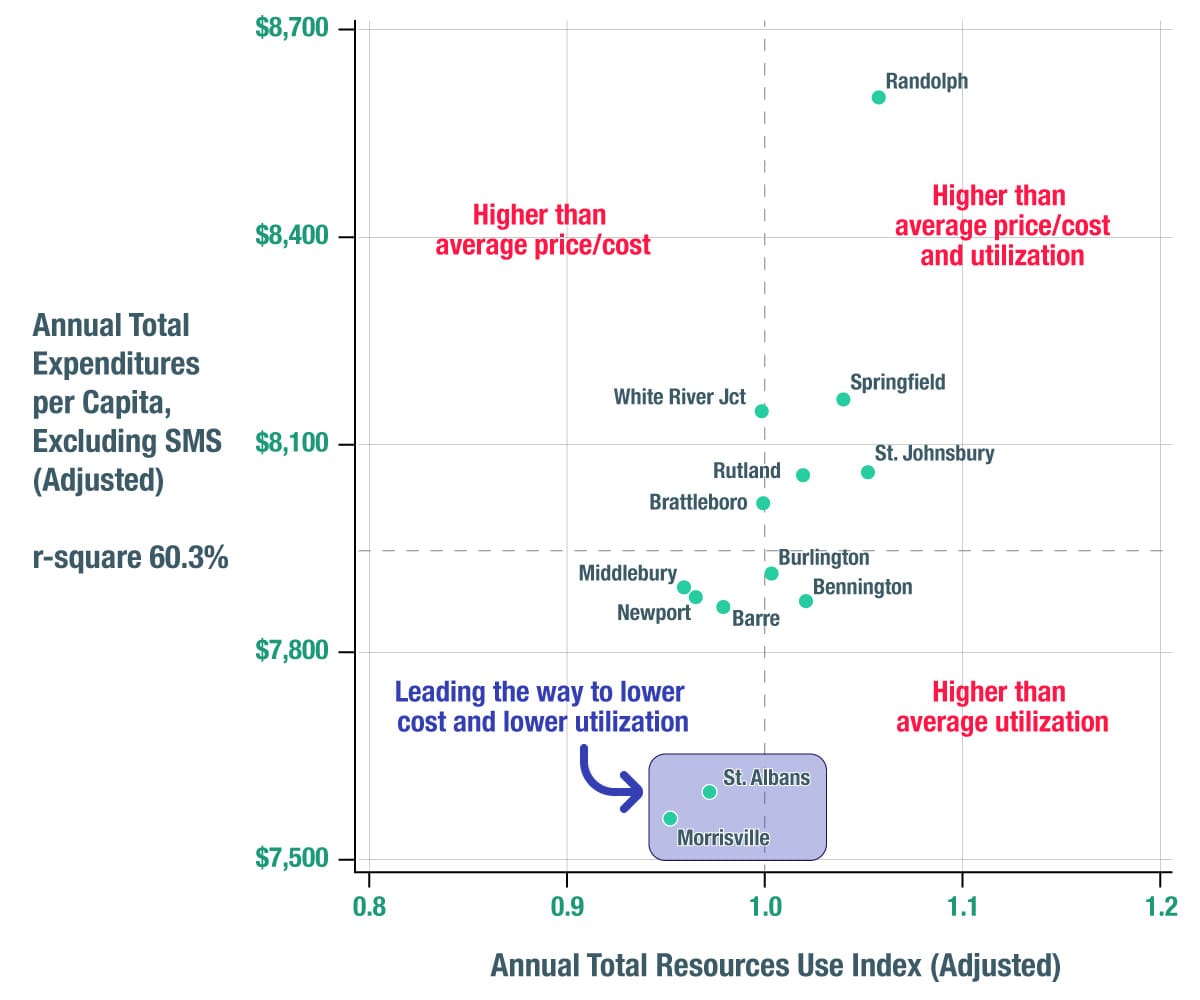
Annual Total Expenditures Per Capita vs. Resources Use Index (RUI)
NMC Achieving the Goals of Healthcare Reform
NMC is a proven leader in the transformation of Vermont’s healthcare system. Our work has helped our service area achieve designation as having lower costs and utilization – the goal’s of healthcare reform – than other areas of the State. Since reimbursements have not caught up with the transformation, this hurt us financially in FY’2019. It is the right path for our community and we will to lead while advocating for reimbursement change and the alignment of priorities and incentives among the Green Mountain Care Board, the Legislature, the Administration, Hospitals, Physicians and Providers, and Payors.
Gifts from Our Community: Annual Donors
Individuals
- Chari Andersen
- Anonymous
- Judy Ashley
- Devin Bachelder
- Doreen Benoit
- Joel Benware
- Leon Berthiaume
- Robert Bessette
- Jonathan Billings
- David Blin
- Richard E. Bombard
- Pamela Bonsall
- John Bostwick
- Paul Bouchard
- Lisa Bovat
- Julia Boynton
- Eric Brigante
- Mark Brooks
- Gregory Brophey
- James Brouillette
- Michele Burke
- Caryn Burleson
- Marie Burleson
- Jerri Bushey
- Mary Bushey
- Michelle Carner
- John Casavant
- Jane Catton
- Amy Centabar
- Elaine A. Charron
- Sandra Chicoine
- Michelle Cioffi
- Brian Clukey
- Kathleen Coburn
- Tom Conley
- Kelly Connolly
- Lisa Cornforth
- Diane Costes
- Robert Cronin
- Heather Cutting
- Donald Davison
- Ann Delaney
- Sarah DeSilvey
- James Dickmann
- Annette Dragoon
- Brian Dubie
- Faith DuBois
- David Ducham
- Kimberly Duffel
- Deborah Durant
- Jeffrey Eaton
- Bonnie Evans
- Amber Felisko
- Hillary Fisher
- Lyle Fleury
- Lydia Foisy
- Sara Frail
- Stephania Fregeau
- Peter Fyles
- Valdemar and Bridget Garibay
- Phil Gerbode
- David P. Gervais
- Cindy Gibson
- Leon Graves
- Christopher Grimes
- Gail Grismore
- Carol Groening
- Marilyn Grunewald
- Amie Hakey
- Amy Harris
- Randy Hartman
- Gerald Herrera
- Christopher Hickey
- William Hobkirk
- Peter Hofstetter
- Kenneth and Judy Holzscheiter
- Jacqui Hood
- Stephen Howe
- Bridget Howrigan Rivet
- David Hutchinson
- Shirley Jacobs
- Robert and Diane Janelli
- John Johnson
- Michael Kennedy, MD
- Edward T. Kissane
- Carol Klette
- William and Bonnie Knaus
- Katharine Laddison
- Molly Lambert
- Brittany LaPan
- Erin LaRocque
- Wendy Lawrence
- Deeanna Lefluer
- Alex Lehning
- Valerie Lehouiller
- Maurice L’Esperance
- John Livingston
- Jean M. Lowe Trust
- Jacy Lunna
- Shirley Lunna
- Tina Machia
- Elaine Magnan
- Katy Magnuson
- Kevin Manahan
- Linda Martell
- Patricia M. Martin
- Haskell Mayo
- Vaughn Mays
- Janet McCarthy
- Mark McGinn
- Mark McGinn
- Jackie McNall
- Kimberly Melhuish
- Jamie Merchant
- John Minadeo, MD
- Paula Minch
- Jeffrey Moreau
- Rev. Moretti
- Kelly Morley
- Sarah Mutrux
- Gerald Myers
- Dr. Joseph and Judy Nasca
- Jonathan Newhard
- John Newton
- Paul Newton
- Sarah Nielsen
- Keirsten Nulph
- William O’Connor
- Judith Olsen
- Mary Ostrander
- Pam Paradee
- Dean Pelkey
- Christine Pignona
- Jamie Pinkham
- Robert Pitts, MD
- Sherry Pontbriand
- David Powell
- Jane Brooks Zurn
- Rampersad
- Peter Rath
- Lester Ravlin
- Prescott Reiner
- Helene R. Richard
- Darrin Ries
- Susan Roberts
- Karyn Rocheleau
- Carl Rosenquist
- Gary & Cindy Rutkowski
- Barb Sargent
- Sherry Scott
- Albert and Sally Severy
- Meagan Shine
- Frank Short
- Frank Short
- Gregory Silvestri
- David N. Simcoe, DO
- Heather Skilling
- Tim Smith
- Sarah Sterling
- L. Lowrey Sullivan, MD
- Thomas Suppan
- Raymond Sweeny
- Lynne Tetreault
- Lindsay Thieken
- Adam Thompson
- Lester Thompson
- Deb Timmerman
- Jill Torrey
- Heather Tremblay
- Madalyn Tulip
- Rod Vallee
- Matthew Walker
- Erin Ward
- Mark Waterhouse
- Lisa Anne Weaver
- Diane Weishaar
- Marie Anne West
- Deborah L. Winters
- Katherine P. Wise
- Deborah J. Witter
- Mary Woodhouse, MD
Businesses & Organizations
- A.N. Deringer, Inc.
- American Legion Green Mountain Post #1
- Bellows Free Academy Student Activities
- Ben & Jerry’s
- Bernstein Private Wealth Management
- BerryDunn
- Brady and Levesque Families
- Casella Waste Systems, Inc.
- Community National Bank
- Community Partners Classic
- Dickinson & Branon Dental Care
- Dickinson & Branon Dental Care
- Fiddlehead Family Dental
- First Response Labor
- Florida Research Instruments, Inc
- Franklin County Industrial Development Corporation
- Franklin County Quilters Guild
- Grady’s Golden Goodness Fund
- Handy Toyota / Handy Chevrolet
- Hannaford Charitable Foundation
- Hickok & Boardman Insurance Group
- Holy Trinity Episcopal Church
- IBM International Foundation
- J&L Service Center, Inc.
- John Leclair Foundation
- Knights of Columbus (St. Albans Council #297)
- McCuin Fuels, Inc.
- Med Associates
- Missisquoi Valley Union High School Student Activities
- MRC Mega Realty Center
- New England Federal Credit Union
- NFP Property and Casualty Services, Inc.
- Northwestern Pediatrics
- People’s United Bank
- Peoples Trust Company
- Rotary Club of St. Albans
- Suncrest Health Care Communities
- The Tyler Place
- The WaterWheel Foundation
- Union Bank
- Vermont Community Foundation
- Vermont Precision Tools, Inc.
- Veterans Valet Service
NMC By The Numbers

Admissions
Lab Tests Run
Diagnostic Imaging Tests
Specialty Practices Visits
Urgent Care Visits

Births

Primary Care/Peds Visits
Assisting All Of Our Patients
Northwestern Medical Center complies with applicable Federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex. Northwestern Medical Center does not exclude people or treat them differently because of race, color, national origin, age, disability, or sex.
Northwestern Medical Center:
- Provides free aids and services to people with disabilities to communicate effectively with us, such as:
- Qualified sign language interpreters
- Written information in other formats (large print, audio, accessible electronic formats, other formats)
- Provides free language services to people whose primary language is not English, such as:
- Qualified interpreters
- Information written in other languages
If you need these services, contact: Jamie Pinkham
If you believe that Northwestern Medical Center has failed to provide these services or discriminated in another way on the basis of race, color, national origin, age, disability, or sex, you can file a grievance with:
Jamie Pinkham
Northwestern Medical Center
133 Fairfield Street
St. Albans, Vermont 05478
802-524-5911, TTY 800-253-0191
You can file a grievance in person or by mail, or email.
If you need help filing a grievance, Jamie Pinkham is available to help you.
You can also file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights, electronically through the Office for Civil Rights Complaint Portal, available at U.S. Department of Health and Human Services Office for Civil Rights, or by mail or phone at:
U.S. Department of Health and Human Services
200 Independence Avenue, SW
Room 509F, HHH Building
Washington, D.C. 20201
1-800-368-1019, 800-537-7697 (TDD)
Complaint forms are available Here